Non-Invasive Cardiology
Specialty > Subspecialty > Non-Invasive Cardiology
Non-invasive cardiology is a branch of cardiac sciences that focuses on diagnosing and treating heart conditions without surgical interventions. It includes various imaging procedures, diagnostic tests, and advanced technologies through which non-invasive cardiologists can check and assess the structure and working of heart. Through these techniques, they can also identify abnormalities and create treatment plans to effectively manage various cardiological complications.
Aayush Hospitals provides comprehensive non-invasive cardiology treatments in Gujarat. Our team of expert non-invasive cardiologists are experts in a wide range of non-invasive approaches to provide accurate and effective cardiac care.
At Aayush Hospitals, we understand the importance of exact diagnosis and analysis of heart conditions. Hence, we are equipped with state-of-the-art imaging technology to provide excellent cardiac care.
What sets us apart from others is that we harness technology along with a team of experts. In addition, our multidisciplinary approach to cardiac treatments makes us the best hospital for cardiac treatment in Gujarat.
An implantable cardioverter defibrillator or ICD is a device to treat abnormal heart rhythms with the help of electrical impulses.
What is an ICD?
An ICD is a life-saving cardiac device that fixes abnormal and fast heart rhythms. It does so by sending electrical impulses to the heart, slowing down the fast heart rhythm, and returning it too normal.
The device is made up of 2 components; defibrillator and leads. It is inserted in either the right or left side of your chest to monitor the heart rhythm for 24 hours/day.
Why Do You Need an ICD?
A healthy heart equals a healthy and steady rhythm. In some people, however, this rhythm can be disturbed and may either beat too fast or too slow which is known as arrhythmia. It occurs due to:
In addition, you could also be at risk of arrhythmia if you had coronary artery disease or heart failure before.
What are the Risks of Having an ICD?
Every surgery involves little or no risk and thus defibrillator also poses certain risks. Although there are no major risks a little bruising or swelling at the site is common. Other lesser common risks include:
What Happens During an ICD?
A defibrillator surgery is conducted in an electrophysiology lab. The best heart specialist in Gujrat will attach you to heart monitors and insert a cannula in your vein. During your surgery, you will be:
After the procedure, you may notice a bulge under your skin at the place where the ICD would be inserted.
What Happens After an ICD?
After the surgery, you will be moved to a recovery area. Our doctors will analyse your condition and give you specific instructions to manage your wound. You may feel tenderness, soreness, or some bruising at the site. This, however, is transient and goes away within a few weeks.
A pacemaker is a small device that helps maintain a healthy heartbeat through electrical impulses.
What is a Pacemaker?
A pacemaker is a small device that helps in maintaining a healthy heartbeat with the help of electrical impulses. The device is made up of battery and leads which are placed under the skin on the left or right side of your chest. It sends electrical signals to your heart to help it beat at a normal rate as well as help in increasing your heartbeat with exercise.
Why Do You Need a Pacemaker?
The best cardiac specialist in Gujrat will recommend a pacemaker if you have abnormal heartbeats called arrhythmia. Arrhythmia may occur due to:
What are the Risks of Pacemaker?
Although pacemakers are generally safe with lesser risks, you may, however, experience some bruising or swelling at the site. Other lesser common risks include:
What Happens During Pacemaker Surgery?
A pacemaker surgery is conducted in an Electrophysiology lab. Before starting the surgery, our doctor will attach you to heart monitors and insert a cannula in a vein in your arm. During the procedure, our doctor will:
After your surgery, you may notice a bulge under the skin where the pacemaker has been inserted.
What Happens After Pacemaker Surgery?
After the surgery, you will be moved to a recovery area. You may observe a little tenderness, soreness, or bruising at the site of the surgery. This is, however, transient and will go away within a few weeks.
Cardiac resynchronization therapy or CRT or Biventricular spacing is a procedure to implant a special pacemaker.
What is CRT?
CRT is a procedure to implant a special or permanent biventricular pacemaker. A biventricular pacemaker helps people contract both their ventricles at the same time.
Unlike a regular pacemaker, a biventricular pacemaker consists of three leads. One lead goes to each of your ventricles and the third goes to your right atrium or one of the upper chambers of your heart.
These leads check for any abnormality in the heart rhythms and send electrical signals to correct them.
Why Do You Need a CRT?
Patients with irregular heart rhythms whether too slow or too fast may require a CRT. Arrhythmia may occur due to:
What are the Risks of CRT?
Although CRT is an effective and safe procedure, you may experience certain risks including:
What Happens During a CRT?
A CRT surgery is conducted in an Electrophysiology lab. Before starting the surgery, our doctor will attach you to heart monitors and insert a cannula in a vein in your arm. During the procedure, the best heart specialist in Gujrat will:
What Happens After a CRT?
After the surgery, you will be moved to a recovery area. You may observe a little tenderness, soreness, or bruising at the site of the surgery. This is, however, transient and will go away within a few weeks.
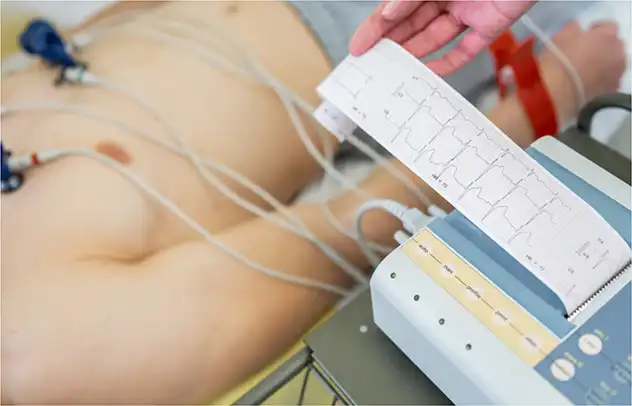
Echocardiography refers to capturing an ultrasound of your heart.
What is an Echocardiograph?
An echocardiograph or simply an “echo” refers to the ultrasound of your heart. An Echo captures the sound waves from your heart to create a detailed account of heart chambers and other structures.
Echo is of the following types:
Why Do You Need an Echo?
A heart specialist in Gujrat will recommend an echocardiography if you have symptoms of:
Heart murmurs.
Heart failure.
Congenital heart defects.
Your echo results will provide information such as:
How your heart muscle is pumping.
Size of your heart.
How your heart valves are working.
If there are any blood clots inside your heart.
If there is any fluid around your heart.
If there are problems with your heart’s blood vessels including the aorta.
What are the Risks of an Echo?
Echocardiography is a safe and painless procedure with minimal risks. In the case of TOE, you may just experience soreness in the throat after the procedure.
What Happens During an Echo?
During the normal Echo procedure:
Some sticky dots will be attached to your chest to monitor heart activity.
The gel will be applied to the chest.
A probe or transducer will be moved around on your chest.
Our doctor may also ask you to hold your breath and lie on your side.
Images of your heart will be recorded on a computer screen.
During TOE, you will be certain medication to relax. The back of your mouth will also be numbed before placing a tube with a transducer into your throat.
What Happens After an Echo?
If you do not experience anything unusual, you can resume your activities immediately after an echo. In the case of TOE, you will be moved to a recovery room and watched for a few hours to let the numbing medication wear off. You will also be asked to take a sip to check if you can normally eat or drink.
Stress testing is a means to identify how your heart responds during times when it’s working at its peak, that is, during or just after an exercise.
What is Stress Testing?
Stress testing also referred to as exercise stress test helps our doctor in determining how well you respond during or just after exercise. The test is either done while walking on the treadmill or pedalling on a stationary bike while attached to an EKG monitor. The responses captured on the screen help our doctor by measuring:
Blood pressure.
Heart rate.
Electrical activity in your heart.
Oxygen levels.
Why Do You Need Stress Testing?
You may be recommended a stress testing in case of:
Congenital heart disease.
Coronary artery disease.
Congestive heart failure.
Heart valve disease.
Hypertrophic cardiomyopathy.
In addition, it is also crucial for pilots or athletes.
What Happens During a Stress Testing?
Stress testing is a safe procedure that takes around up to 30 minutes to 1 hour. During the procedure:
Our best heart specialist in Gujrat will take your normal vitals including resting heart rate and blood pressure.
Small and sticky dots, that is, electrodes will be attached to your chest and arms. The electrodes are connected at one end to the EKG machine.
You will be asked to either walk on a treadmill or pedal a stationary bike at an easy pace.
Over time, our doctor may also ask you to increase the pace to a manageable level.
The test will continue to capture your target heart rate for up to 10-15 minutes.
The test may be halted if you experience severe symptoms or feel dizzy.
What Happens After a Stress Testing?
Once the test is completed, our doctors will monitor your symptoms, heart rate, blood pressure, and ECG until it returns to a normal range. After your heart rate has recovered, you may return home.
A Holter monitor is a device that records your heartbeats.
What is a Holter Monitor?
A Holter monitor consists of electrodes, wires, and a small machine attached to your waistband. This helps in recording your heartbeats.
Why Do You Need Holter Monitoring?
You may require Holter monitoring if our doctor suspects any problem with your heart rate or rhythm. Other reasons include:
Dizziness.
Fainting.
Chest pain.
Shortness of breath.
Arrhythmia or irregular heartbeats.
What are the Risks of Holter Monitoring?
Holter monitoring is a safe procedure with no significant risks. Some people, however, may experience minor skin irritation from the electrodes.
What Happens During Holter Monitoring?
Holter monitoring is a safe, painless, and straightforward procedure during which:
Electrodes will be attached to your chest.
Electrodes will be further connected to a small Holter machine device.
While our doctors fit the device on your waistband, you will need to:
Keep wearing it during your usual activities.
Keep it on at all times including sleep.
Keep a diary and jot down all your daily activities and the time spent on them.
Record any unusual symptoms including dizziness, chest pain, or shortness of breath.
What Happens After Holter Monitoring?
After one or two days of attaching a Holter device, you will be asked to visit Aayush Hospital inGujrat. Our best heart specialist in Gujarat will remove the device, analyse the results, and recommend further treatment.
Ambulatory blood pressure monitoring is a method in which your blood pressure is recorded continuously for straight 24 hours.
What is Ambulatory Blood Pressure Monitoring?
Ambulatory blood pressure monitoring is a procedure that measures as well as manages high blood pressure. The method keeps monitoring your blood pressure for 24 hours whether you are awake or asleep.
The device used for this purpose takes dozens of readings every 15 to 30 minutes during the day and every 60 minutes a night. In addition, it also measures your heart rate.
Why Do You Need Ambulatory Blood Pressure Monitoring?
You may require ambulatory blood pressure monitoring to:
Confirm hypertension.
Identify how change in your blood pressure affects your daily activities and sleep pattern.
See how well your blood pressure medication is managing high BP.
Check the difference in blood pressure readings at the hospital and home.
What is the Risk of Ambulatory Blood Pressure Monitoring?
Although the process is safe and non-invasive, it may seem uncomfortable for some. Other common risks include:
Soreness in the arm.
Skin irritation.
Disrupted sleep pattern.
What Happens During Ambulatory Pressure Monitoring?
Once you visit us at Aayush Hospital, you will receive equipment and instruction for the next 24 hours. Our doctor will attach the equipment to your body and ask you to carry on your usual activities.
Due to continuous BP reading your arm may inflate and squeeze every 15-30 minutes. This may at times also affect your sleep.
What Happens After Ambulatory Pressure Monitoring?
After 24 hours, you will be asked to visit our hospital again, our best heart specialist in Gujrat will analyse your BP readings and discuss further treatment.